I am a psychiatrist at Columbia University Irving Medical Center. I have many great colleagues on the medical side of things who are performing heroically during this pandemic, many of whom I met as a medical intern 15 years ago. The ties we developed during that grueling year are lifelong. I check in with them regularly to see how they are managing during this difficult time and lend an ear when I can. They are all heroes.
One of the people I met as an intern became my best friend. We had the same interests and went to the same church. I introduced him to his wife and got to know his family.
After residency, he moved a few hours away and opened up a practice. Within a short period of time, he was helping thousands of patients a year. He was a top-rated doctor, and his patients loved him. He was sought after by many high-profile celebrities and athletes.
After a few years, we began to speak infrequently, but every time we talked it was as if no time had passed. He always seemed to be in great spirits.
Then I found out on a holiday a few years ago that he had died by suicide. I had no idea anything was wrong.
The Focus on Mental Health Is Warranted
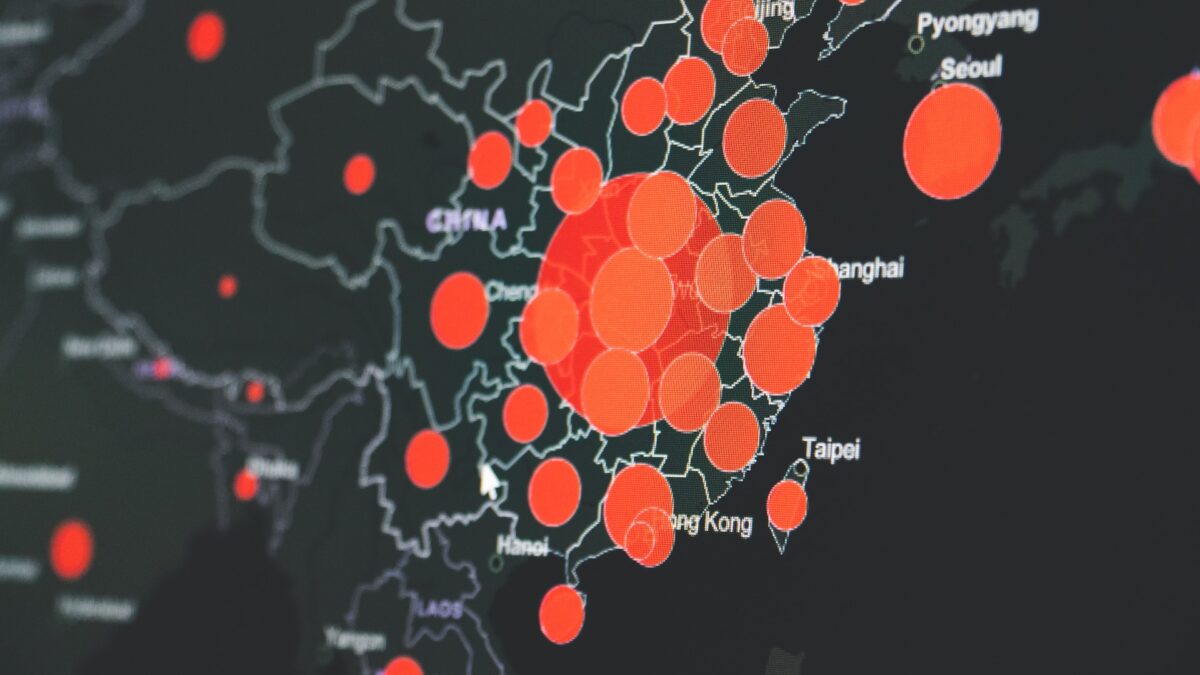
With the vast majority of states in the reopening phase of the Covid-19 pandemic, many in the media and medical field are placing more attention on the looming mental health crisis. Rightfully so. The economic turmoil, isolation, and loss of family and friends have taken and will continue to take a toll on everyone involved.
One group that requires special attention is frontline health-care workers. Few have been more exposed to the horrors of the pandemic.
As a psychiatrist in New York City, I hear about these horrors and their effects on health-care workers from my colleagues daily. Operating rooms and wings of hospitals are used as makeshift intensive care units with seemingly endless rows of beds, occupied by patients on mechanical ventilators. Minimal visitors are allowed. Refrigerated tents stand outside hospitals to store dead bodies. Family members beg to see patients before they die.
Health care workers feel helpless as they see upwards of 80 percent or more of their patients passing. Physicians constantly second-guess their decisions. Physicians and nurses break down in stairwells. Tragically, some are even lost to suicide.
These stressors and conditions are over and above the already higher rates of suicide, self-medication, substance use, and depression and other psychiatric disorders among physicians, as reported by the American Foundation for Suicide Prevention. The situation is especially dire for younger physicians, such as residents, many of whom are shouldering the load at hospitals in harder-hit areas.
Having had several of my physician colleagues and very close friends commit suicide over the past several years, I can personally attest to these harrowing realities. The pandemic is only going to make things worse. Therefore, in addition to addressing the severe, upcoming crisis of mental health issues in general, we must be quite specifically prepared for the mental health problems we will see in frontline health-care workers.
Fortunately, there is hope. Despite what many people believe, mental illness is usually very treatable. Nowadays, we have medications that work with minimal side effects. A number of different psychotherapies are evidence-based and can be used to treat a variety of disorders. For many disorders, the combination of medications and therapy works best.
The revolution in telehealth has made mental health treatment available to more people than before. Policymakers and insurance companies are doing what they can to encourage the use of mental health services, especially through telehealth.
Help Health Care Workers Get the Support They Need
In addition to these individual treatments, many crisis lines are available to help people who need to reach out. The American Medical Association encourages and recommends support groups and workload redistribution.
These interventions and others will help, but they only help people who take advantage of them. Unfortunately, the adage that “doctors are the worst patients” is as true for mental health as it is for physical health.
Physicians are often burdened with unnecessary expectations of stoicism. Many revert to denial or may simply not have enough time to seek out treatment. Others may experience the stigma about mental illness that still pervades the medical field and the rest of society, or simply feel uncomfortable sharing their feelings.
There will be no one-size-fits-all strategy for dealing with the mental health of frontline workers. It will be incumbent upon policymakers, hospital administrators, training directors, and, ultimately, individual health-care workers themselves to break down institutional, financial, systemic, and personal barriers to the receipt of adequate care for frontline workers, such as physicians and nurses.
Importantly, one cannot forget non-medical personnel who work in health-care settings, such as food service workers, housekeeping staff, security, and others who are indeed essential. These people are often exposed to as much death and dying as the health-care workers and may be just as vulnerable to adverse mental health outcomes.
Depression, substance use, and suicidality can affect anyone. We must all remain vigilant and proactive about potential signs or symptoms in our colleagues, friends, and family. Almost everyone has a close family member or friend with mental illness, whether you know it or not.
Mental illness is treatable and is not a sign of moral weakness. In my experience, people who are depressed or suicidal often don’t just share their feelings uninvited. However, they are almost invariably willing to talk about their feelings if asked in a sincere, nonjudgmental way.
I just wish I could have saved my friend.