Americans, who practices medicine on you? The answer may seem self-evident, but it is not. In our current health-care system, millions of nameless, faceless government or private insurance bureaucrats practice medicine on you without a license for medicine.
You may think your life is in your doctor’s hands, but it is not. The bureaucrats, not you or your doctor, make your medical and financial decisions. Consider these health-care decisions:
- Diagnosis
- Treatment: what, when, where, by whom
- Medications
- Paying for care
Your doctor does not express your diagnosis in words such as arthritis, asthma, or heart failure. If a physician or hospital wants to be paid, they must use a letter-number diagnosis listed in the International Classification of Disease (ICD-10) code book, which turns 1,400 human ailments into more than 68,000 codes. Examples of these “diagnoses” include: W55.21 (bitten by a cow); W61.33 (pecked by a chicken); V00.01 (pedestrian on foot injured in collision with roller blader); Z63.1 (problem with in-laws); and my personal favorite, Y92.146 (injured at a swimming pool within a prison).
Once a diagnostic code is established, you expect the doctor to recommend the correct treatment by the most experienced operator in the best facility at the optimal time given your medical condition. In reality, you will receive whatever the insurance carrier allows, whenever the carrier allows it, at a contracted facility, by a specialist on the insurance carrier’s panel. All those medical choices are made by nameless, faceless bureaucrats, not your personal medical caregiver.
Doctors Don’t Get to Make the Decisions
Clinical advisories and guidelines written by federal administrators have become medical mandates. These treatment plans generally work well for large populations but do not allow for the specific idiosyncrasies, variations, or allergies of individual patients that only their personal physicians know. Although wanting the best care for you, if the doctor deviates from the approved treatment plan, he or she risks reprimand, financial penalty, and even loss of clinical privileges.
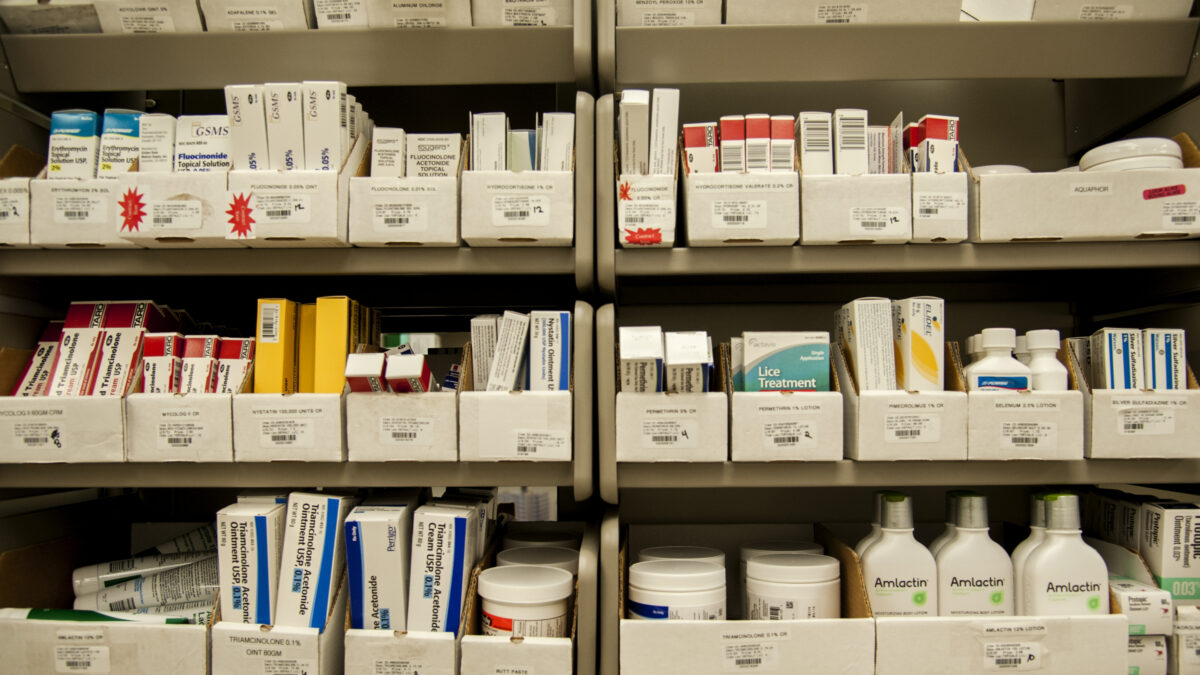
Since you watched your doctor write your prescription, you assumed he chose your medication. Reality is otherwise. The medication you get is decided by a pharmacy benefits manager (PBM), a company contracted by the insurance carrier or health plan. Only the drugs listed by the PBM are available to the prescribing doctor, based on step therapy.
Also known as fail first, step therapy starts with drugs that have the cheapest price, largest rebate to the PBM, and least risk of adverse reaction. These are the drugs the doctor can prescribe, even if they are not the right medications for you. Only after you have taken them and after the doctor proves to the PBM that the medication failed, can a second, stronger set of drug options become available. Eventually, the PBM may allow the doctor to prescribe the drug he or she wanted for you in the first place.
Recall the promise, if you “like your doctor, you can keep your doctor,” assuring patients they could choose their doctors. While the doctor shortage before 2010 did limit patients’ options for personal physicians, the Affordable Care Act further reduced the possibility you could have the doctor of your choosing in the following way.
Obamacare raised costs to all insurance companies by expanding eligibility and benefits, reducing medical underwriting, and increasing administrative burdens. Insurers offset the increased expenses by narrowing their medical panels.
In other words, they fired physicians, eliminating them from their contracted panels. Privately insured patients were forced to choose their doctors from a much smaller pool than previously. It is worse for Medicaid patients: Nationally 31 percent of physicians do not accept Medicaid patients, and in Texas, less than half do.
Third Parties Determine Health-care Outcomes
Money is an incentive used to reward preferred behaviors and outcomes. “He who has the gold makes the rules.” In health care, he who controls the money determines what is preferred. As third parties rather than consumers decide what your doctor is paid, third parties rather than consumers determine the outcome. As a result, the outcome is not timely care.
Covering 180 million Americans, private insurance companies’ preferred outcome is profit. The longer they withhold payment, the more money they make. Thus, insurance carriers delay, defer, and deny patient care.
The federal government is the third-party payer for 140 million Americans through Medicaid, Medicare, and Tricare. Washington’s preferred outcome is extension of its power. This is accomplished by expansion of the scope and reach of the federal bureaucracy.
To pay the exorbitant costs of federal bureaucracy, Washington diverts money from providers and hospitals to pay bureaucrats and agencies. As a result, patients have less access to care and longer, medically dangerous wait times before they can see a doctor. Some even die waiting in line for life-saving care.
With the current third-party payment structure, you doctor does not practice as much medicine on you as insurance executives and federal bureaucrats do. As a result, Americans do not get timely needed care. The only way for patients to get the care they need when they need it is to restore a direct doctor-patient relationship, without a third-party payer in between making medical and financial decisions.
Someone will no doubt exclaim, “I can’t possibly afford to pay for my care.” The proper response is, “Last year, you did pay $28,166 — what did you get for it?!” If each patient were in control of family health-care spending, the United States could have a free market for health-care goods and services.
Prices would plummet. Add safety nets for the “disabled, blind, and aged,” the originally intended Medicaid population, and all Americans would have the health care they want: affordable and accessible.