The University of Nebraska Medical Center (UNMC) in Omaha may be skirting laws governing the procurement of human organs for transplant by harvesting organs from individuals who may not yet be dead.
UNMC surgeons have developed a protocol for “normothermic regional perfusion with controlled donation after circulatory death,” a practice fraught with ethical concerns.
Under UNMC’s protocol, published at clinicaltrials.gov, the donor is removed from life support, and once the heart has stopped (circulatory death) the surgeons wait five minutes – as required by Nebraska law – to see if the heart restarts on its own.
If it does not, surgeons cut open the chest cavity to begin organ harvest, then sever blood flow to the brain – ensuring brain death – before artificially reanimating the circulatory system with an external pump. The resumption of blood circulation restarts the beating of the heart, keeping the organs functioning and viable for harvest.
In 1981, the Uniform Determination of Death Act (UDDA) became law, establishing the parameters by which an individual may be considered “dead.” As per the law, a person may be declared legally dead after the “irreversible cessation of circulatory and respiratory functions, or the irreversible cessation of all functions of the brain, including the brainstem.”
UNMC’s restarting of the circulatory process within minutes of declared death proves the circulatory and respiratory functions have not “irreversibly” ceased. Proponents of UNMC’s organ harvest protocol dismiss this apparent contravention of the UDDA by claiming the donor is “brain-dead” by the time circulation is resumed.
What isn’t acknowledged is the harvester’s role in bringing about that brain death, caused by their own interruption of the brain’s blood supply, as described in the second step of UNMC’s protocol:
2) Ligation of all the blood vessels that supply blood to the brain to ensure that blood flow to the brain is not reestablished once circulation is restarted as described below.
If the brain is already “dead” as claimed, resuming blood flow would not bring it back, making this step unnecessary. The fact the step is included reveals the brain may indeed still be functioning at some level, and the organ harvesting surgeons know it.
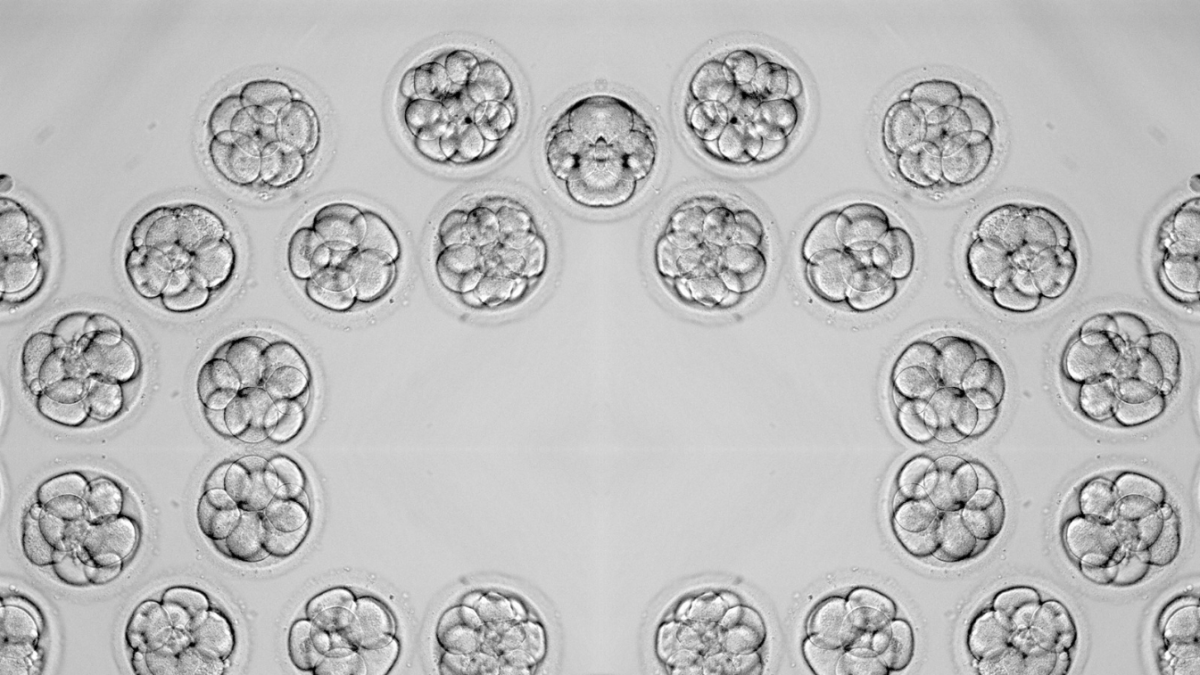
The intent of this macabre procedure is to preserve the body’s organs as close to living form as possible.
Further consideration gives rise to an unthinkable horror. According to the protocol, the opening of the chest occurs in step one, before cross-clamping the blood supply to the brain. It is therefore possible the donor is aware of what is happening to them.
Considering organ procurement teams use no anesthesia during these procedures, the possibility the patient may be aware, even dimly, of the violence done to their body is horrifying.
Brain-dead organ donors frequently release catecholamines during organ procurement. Catecholamines are hormones produced by the brain, nerve tissues, and adrenal glands in response to severe emotional or physical stressors, suggesting at least some level of sensory awareness remains.
While some medicos may see this procedure as a clever means of circumventing the “dead donor rule,” (which forbids the killing of a donor by the act of harvesting their organs or tissues) many other medical professionals are extremely uncomfortable with this process, pointing to frequent instances of spontaneous resuscitation long after the five-minute waiting time observed by the UNMC harvesters.
Dr. Heidi Klessig, a board-certified anesthesiologist specializing in pain management writes, “Dr. Ari Joffe, a clinical professor of pediatrics and critical care at the University of Alberta, has found at least 12 patients whose hearts restarted without any medical intervention after as much as 10 minutes of cardiac arrest, and some of these patients made a complete recovery.”
Klessig gave a further example. “In 2020, the heart of a young woman who had been declared dead by circulatory criteria was noted to have restarted during the removal of her kidneys, as she began to gasp for breath.”
Upon recognizing her spontaneous resuscitation, attending physicians administered an unusually large dose of fentanyl, which killed the patient. Her “second” death was declared a homicide by the coroner.
As UNMC’s protocol involves the death of a donor at the hands of a physician for the purpose of organ harvest, it appears to be a clear violation of the dead donor rule despite the semantic dance performed by protocol advocates.
Given the ambiguity surrounding this method of organ retrieval, the American College of Physicians (ACP) recommended in 2021 that the practice be halted, as “the burden of proof regarding the ethical and legal propriety of this practice has not been met.” Australia has banned this method of organ harvest altogether.
UNMC’s published study coincides with a movement openly calling for the abandonment of the dead donor rule. Robert M. Sade, professor of Surgery, Chief of Section of Bioethics in Cardiothoracic Surgery, and the Director of the Institute of Human Values in Health Care at the Medical University of South Carolina, writes:
The facts that brain-dead patients are not really dead before organs are recovered and that DCD donors are imminently dying but not yet dead means that current practices of organ donation from both brain-dead and DCD donors are not consistent with the DDR, yet these practices are ethically and legally well-grounded. Once this is recognized and accepted, the DDR, being neither a statute nor a regulation, can be discarded and physicians need not feel as though they are ethically or legally at fault.
Dr. Sade is not alone in his utilitarian worldview. Scholarly articles calling for abandoning the dead donor rule have increased dramatically in the last decade.
However, noted medical ethicist Dr. Doyen Nguyen, a pathologist and specialist in neurosurgery counters those arguments by reminding her colleagues the dead donor rule is the primary ethical bulwark against treating human beings as transplantation farm stock.
She is at the vanguard of those insisting the dead donor rule and the Uniform Determination of Death Act must not be “reformed” with an eye to increasing the organ donor pool, lest the public trust in the medical declarations of death be eroded, and along with it, America’s trust in the very concept of organ donation.
As Dr. Klessig concludes, “Transplant physicians who perform [UNMC’s protocol] are playing fast and loose with both the spirit and letter of the law as spelled out by the Uniform Determination of Death Act. How many families would give their loved ones over to transplant teams if they knew the grisly reality taking place behind the operating room doors?”
Debates like this occur outside of general public view, among myriad physicians and researchers writing in arcane medical and scientific journals. However, the decisions that come about from these discussions are later published as updated guidelines that eventually find their way into law.
UNMC is a taxpayer-supported institution. In politically conservative Nebraska, it’s unlikely residents will consider this an acceptable use of their tax dollars.
Dismissing the physician’s charge to “first, do no harm,” will further erode the public’s trust of medicine, a trust already battered and bleeding from the self-inflicted blows of the Covid-19 pandemic response.
Worse still, it will likely upend the reputation of organ donation as a collective good, as the entire enterprise devolves into a white-coated brawl over who can grab the freshest organs.
Organ donors must be given the opportunity to reconsider their choice in light of this information. Failing to detail the particulars of this procedure to prospective donors and their families puts the lie to harvester claims of “informed consent.”
Once again, the public is forced to remind science – just because you can, doesn’t mean you should.
Attempts to reach UNMC physicians for comment regarding this procedure remain unsuccessful as of the time of publication.