The Commonwealth Fund has come out with the latest iteration of its ongoing campaign to inform our political leaders (not so much the public) that the American health care system sucks.
Many of my conservative friends have pushed back, arguing that it is Commonwealth’s study that sucks. David Hogberg argues that it would have been more useful to print the study on toilet paper. Avik Roy says it is bogus to base such conclusions on public opinion surveys. And Philip Klein says Commonwealth cherry-picked what it looked at to derive its pre-determined conclusion.
Personally, I agree with all of the above. Yes, Commonwealth’s study is deeply flawed, but so is American health care, which is inefficient, bureaucratic, unaccountable, inconvenient, of questionable quality, and far too expensive. But even Commonwealth doesn’t argue that the European systems are a whole lot better. It points out that some countries are better than others in some aspects, but worse than others in other qualities, and that “in most instances (even) the top-ranked country is performing at less than an ‘ideal’ level.”
In fact, these systems are not as starkly different as is commonly portrayed. Nearly all are a mix of public and private coverage, and in many cases, significant out-of-pocket costs. As the chart from OECD below shows, the United States has one of the lowest rates of OOP spending in the world, as a percentage of total spending. And, while only half of our spending is through public programs, even Canada’s much vaunted “single payer” system includes 27% private spending. 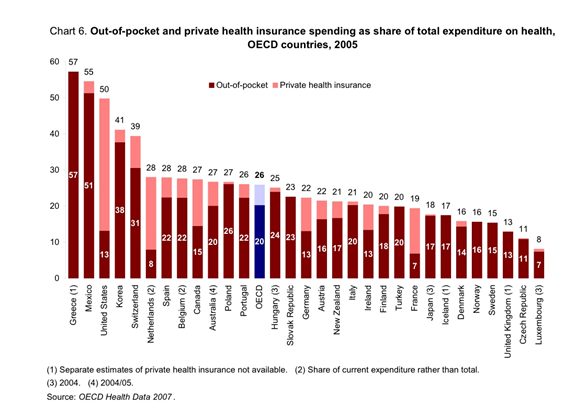 The one big exception for the United States is total cost. Commonwealth places excessive emphasis on costs to bring down the American ranking. In virtually every instance of the U.S. ranking below other countries it is due to the cost of care. For instance, in questions of access to care it reports on the number of people who –
The one big exception for the United States is total cost. Commonwealth places excessive emphasis on costs to bring down the American ranking. In virtually every instance of the U.S. ranking below other countries it is due to the cost of care. For instance, in questions of access to care it reports on the number of people who –
- “Had medical problems but did not visit the doctor because of cost in the past year.
- “Did not get recommended test, treatment, or follow up because of cost in the past year.
- “Did not fill a prescription of skipped doses because of cost in the past year.”
(Bolding mine) Note that it is unconcerned about access denied or delayed for other reasons such as availability of services. One might think that having access to a needed service, even if it costs you something, is far better than not having access at all. But that is not how Commonwealth sees things. It is also unconcerned about how the service is paid outside of direct out-of-pocket spending.
Yes, I may have a substantial copayment in getting a needed treatment, but how much more in taxes would I have to pay to avoid that out-of-pocket expense? Is it more efficient to pay taxes to a government agency, which then pays the provider for the service, or to skip the administrative burden and pay the provider directly? Passing the money through Washington before it goes to the provider means paying many additional people to handle the money.
Surely this cannot be very efficient. Still, American health care is indeed far too expensive — we already know that. But we also know that the United States is a very big, messy, and extremely diverse country. We have four times the population of the next biggest country examined (Germany) and 30 times the landmass, and while Germany’s population is homogeneous (93% are ethnically European), America includes very large proportions of Latinos, Asians, African Americans, and new immigrants. There are costs involved with managing all this that none of the other comparison nations are subject to.
The Commonwealth analysis of “Effective Care” deals solely with prevention and chronic care management. It has nothing at all to say about acute care services, where the U.S. excels. Even its measures of prevention all amount to just talk, not actual results. It includes things like whether “the doctor or other clinical staff talked with (the) patient about a healthy diet and healthy eating” and whether “patients receive reminders for preventive care.” Remarkably, the Commonwealth report states, “The widespread and effective use of health information technology (HIT) in the U.K. plays a large role in the country’s high score on the chronic care management indicators….” Is this the same U.K. that just wasted $12 billion on a HIT system that did not work and was completely discarded?
The section on “Coordinated Care” isn’t bad, though it places an inordinate amount of emphasis on whether the patient had a regular doctor when the variation between countries is small (from 100% in the Netherlands to 91% in the U.S.) and it notes that only 57% of Americans have had the same doctor for five years or more. That shouldn’t be surprising given the mobility of Americans and our unique tendency to move frequently. It is hardly a problem with the health care system. The section on “Efficiency” is almost entirely cost related. It says, “To measure efficiency, this report examines total national expenditures on health as a percent of gross domestic product as well as the percentage spent on health administration and insurance.”
I’m not sure this is particularly good measure of efficiency, but we’ve already stipulated that the American system includes a great deal of waste and is not very efficient. It is the section on “Equity” that is the most problematic. The report cites the Institute of Medicine definition of equity as “providing care that does not vary in quality because of personal characteristics such as gender, ethnicity, geographic location, and socioeconomic status.”
But then it looks solely at comparisons based on income. Granted this is much easier to measure than the other factors, and that some of the other factors are dubious to begin with. Location, for instance –obviously someone living close to the great research hospitals in Boston or Baltimore will have access to higher quality care than a farmer in North Dakota. But even in comparing income groups (those with above average or below average incomes), the report is simply not very good, relying completely on patient surveys rather than actual results. One example is the question of whether the patient received “unnecessary duplication of medial tests in the past two years.”
How is the patient to know whether the test was necessary or not? And, if the patient did not receive a necessary test at all, she would answer “no” to this question and Commonwealth would consider that good. Still, thanks to our horrible Medicaid programs, it is true that lower income people get much worse health care than the rest of us. But I doubt if Commonwealth will join me in calling for replacing Medicaid with coverage more like what the rest of us get.
Now, Commonwealth does confess that there are problems with its report, though not until you get to page 27, where it says:
Any international comparison of health care is subject to inherent weaknesses, such as the absence of medical record clinical information or timely health outcomes data. The measures, methods, and data used in this analysis are far from perfect. Different measures, moreover, are given equal weight in the rankings and are not weighted based on independent evidence of what patients value most highly.
Unfortunately, very few reporters will get to page 27 to see the disclaimer. Instead they will rely on the press release, or the Executive Summary (if they are really diligent) and draw the conclusion Commonwealth wants them to draw: America sucks, and here is the proof!