Bobby Jindal wrote this fall in National Review about “Preventing Single-Payer,” emphasizing that without a better policy proposal, advocates of single-payer health care will eventually win the argument. My family’s experience shows how catastrophic that would be, yet provides a way to transition toward a system that promotes lower costs and increased medical freedom.
We’ve had a lot of medical bills the past several years. I had a broken arm, which required surgery and a plate to mend, my wife suffers from hypothyroidism, with periodic doctor visits and lab tests, and my 20-year-old daughter has been dealing with debilitating Lyme disease-like symptoms for three years before we found a doctor who would prescribe enough different antibiotics long enough to cure it. Her symptoms included muscle and joint aches, fatigue, a low-grade fever, points of tenderness that hurt when touched, sore eyes, and other things that made normal life difficult.
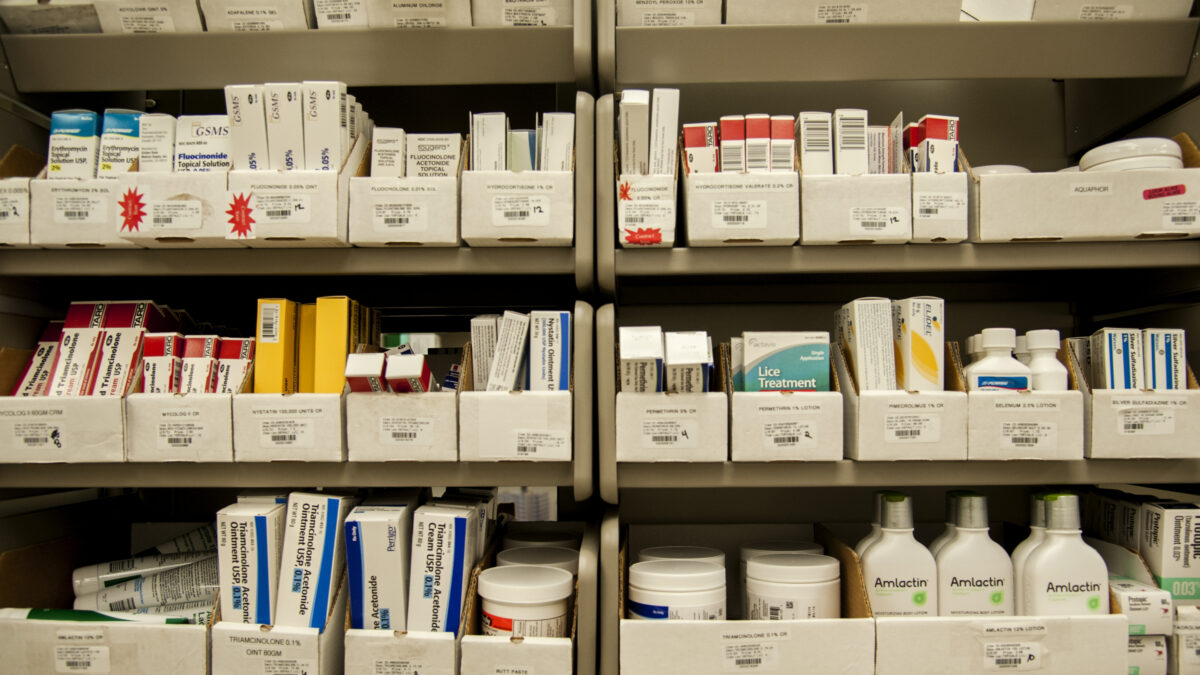
This led to stacks of medical bills not paid by insurance and mailed weeks or months after each test or medical visit, even after we first paid copayments with a health savings account (HSA) card. Those bills, and the thick insurance “explanation of benefits” (EOB) paperwork that tells what our insurance company will pay while claiming credit for negotiating a discount, caused me to think about what a better system might look like.
Is There a Better Way Than Paying Through Insurance?
Paying through insurance raises medical prices and rations care. This is explained here, here, here, and here. One medical provider told us that if we paid ourselves and not through the insurance company, they would cut the bills in half! In our meeting with them, they showed us a two-inch-thick stack of paper from the insurance company for our case that obviously cost money to produce and to have their staff read.
One study estimated that administrative costs were 25 to 31 percent of total health care expenditures in the United States, much higher than other developed OECD countries and growing faster than other health costs. But while some doctors offer substantial discounts for cash payments, just Google “price gouging uninsured patients” to see thousands of articles where paying yourself costs more.
Some hospitals overcharge by 1,000 percent for uninsured or out-of-network patients for whom insurance doesn’t negotiate prices, and they don’t tell you the costs in advance so you can shop around. For emergency treatment, there isn’t time to choose the ambulance and hospital. There are a few ways to make cash king, though, and to tackle some of these problems throughout the country.
First, require lower medical prices and insurance premiums when bills are paid at the time of visit with cash, debit card, or check, without the medical provider filing insurance claims forms or waiting for payment. The cash prices would be lower than what the provider now gets from any private insurance company and could be disclosed ahead of treatment, or service would be free.
This would bring price transparency, competition for price and reputation, and the resulting efficiencies of not submitting all payments to insurance. People could now avoid overpriced doctors, hospitals, and treatments. The price would be higher when paying with credit card, deferred payment, or an insurance company that is billed. During the transition where some insurance plans still pay as they do now, any time a medical provider accepted a lower insurance payment it would also lower the cash price for everyone else.
Outsourcing to Banks
Second, the bank could manage your HSA and become a trusted intermediary between you and the insurance company, billing insurance to repay your account after the deductible is reached. This revolutionary step automates collecting from insurance after making cash payments without you filing each claim yourself, and banks can offer new financial services to make this extra work worthwhile. Since banks already handle debit cards, they can make insurance claims easy so people can save 30 to 50 percent paying cash and not miss the convenience of the current system.
Since they would be dealing with multiple insurance companies on behalf of many customers, banks can tell which ones pay promptly so customers can then switch insurers. Like with online bill payments, the bank would know your insurance company’s electronic number to submit monthly payments and bills, what your deductibles, copayments, and out-of-pocket maximums were, which items your plan covers, and the reimbursement rates for each. The insurance company would provide these rules in a form the bank’s computers could check automatically, saving them money in order to lower premiums.
Insurance companies that refused to submit this information would be required to reimburse 80 percent of any medical cost after the deductible, and 100 percent after the out-of-pocket maximum. Pre-treatment checks would be simplified to just checking this list at your bank.
All medical expenses potentially covered by insurance have an ICD-10 or similar code. The bank would get the list of non-covered codes from the insurance company based on the personalized plan the policy holder selected, with cheaper insurance plans excluding more codes or having other limits. When billing the insurance company, the bank’s computers would only count covered items after the deductible was reached, then subtract copays, and for efficiency send the insurance company bills in batches for groups of customers after some dollar or time threshold was reached.
The insurance company would be obligated to pay the bank’s bill in full, with no EOBs to explain why they didn’t pay. This way the bank keeps the payment details private while the insurance company only knows the amounts it has to pay without knowing which tests, treatments, or medications each person received. You would regain your patient privacy (since the insurance company would know the cost but not your medical file, and cannot send you intrusive questions after treatment, or interfere with doctor-ordered treatment). Ideally, banks would get a full bill electronically from the provider so that as you look at your HSA or bank account online, you can click to see the details of each bill.
Third, legalize new health care financial services so banks can set up separate divisions to offer medical insurance as stiff competitors to existing insurance companies with better prices, customized plans, and service. Along with other companies competing with existing insurance companies, they no longer need to negotiate networks of providers, and now just reimburse patient accounts with effectively a universal network.
For patients, eliminating in-network versus out-of-network distinctions now gives access to the best medical providers instead of limited networks. Banks could also offer overdraft protection for these accounts either from other accounts or as loans. Banks would have detailed price and usage information for customers and could suggest cheaper alternatives for medicine, doctors, hospitals, or laboratory tests.
With this information, you could negotiate lower prices or switch providers to save money. The best HSAs would offer this advice to patients free, but possibly charge referral fees. Banks could also compile anonymized usage statistics into reports that are sold to providers who want to expand their market share.
Clamping Down On Fraud and Abuse
Fourth, authorize private and government lawsuits for pricing fraud where cash prices are not the lowest, or uninsured and emergency patients are overcharged, or for common abuses like upcoding. Use antitrust and Racketeer Influenced and Corrupt Organizations Act (RICO) laws to increase competition. Negative publicity and a reputation rating system can also reduce demand for overpriced hospitals by sending ambulances elsewhere. Banking regulators could enforce the rules so banks don’t misuse their new position.
Fifth, permit medical insurance to become like auto insurance, where claims are infrequent, and much lower premiums are based on claims. Like selecting your auto policy for deductibles, glass coverage, and other items, medical insurance companies should offer personalized plans to cover only what you want instead of forcing you to pay for a bunch of things you don’t need while not paying when you need them to.
This causes people to make coverage tradeoffs based on cost and need, and eliminates insurance reneging on expected payments. It also lowers insurance prices by not forcing everyone to subsidize other people’s treatments for things they don’t want to insure, as proven by short-term plans of 364 days or less that are 80 percent cheaper and Medi-Share-like plans.
Increasing Both Global and National Competition
Sixth, permit pharmacies and other resellers to get the lowest worldwide cash price from U.S. pharmaceutical companies, saving U.S. customers money without reimportation. Like the Foreign Corrupt Practices Act handles bribery, this could end the practice of American companies charging higher drug prices in the United States than overseas even when given the best payment terms.
Seventh, have Medicare and Medicaid operate like other insurance companies using experience like this so that 59 percent of the health care market isn’t left out. Copayments and insurance rates could be lower if payment came from the patient’s account first and then was reimbursed later.
Eighth, make other pro-competition reforms to train more doctors in medical schools and residencies, and eliminate requiring certificates of need before hospitals can be built.
In my daughter’s case, it was an independent doctor not part of a hospital system who provided the right diagnosis and treatment without accepting insurance. Other doctors had been prevented from treating her by insurance companies and their own management. We could see the fear in their eyes and their agitation as they refused to prescribe antibiotics.
Thankfully, my daughter is better now, but she could have suffered a decade or more, with lifetime consequences, had we followed their advice for psychotherapy, exercise, and other “treatments” apart from the antibiotics that cured her. Being able to pay the doctor yourself isn’t just more efficient, or only for difficult illnesses like Lyme disease. Sometimes it saves lives because you now have access to doctors and treatments your insurance would have denied you.
Preventing single-payer isn’t about denying care to those who need it; it’s all about increasing medical freedom for those who need it most.