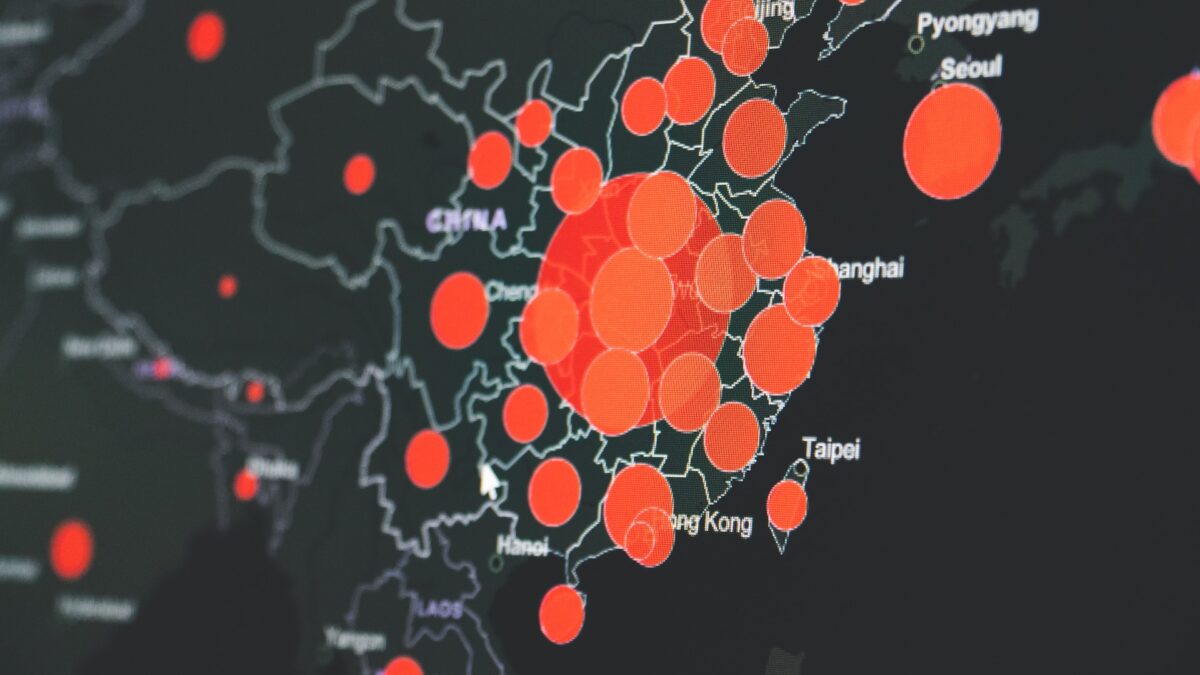
Nursing homes and their occupants currently account for more than 43 percent of all coronavirus fatalities in the United States as of May 26, according to Forbes. Reporting from the New York Times detailed that by May 11, COVID-19 had already infected more than 153,000 patients at over 7,700 facilities nation-wide.
While that statistic demonstrates the widespread nature of the crisis, what’s more alarming is that by the date of the New York Time’s analysis, only 11 percent of total US COVID cases originated at nursing homes, but over 35 percent of the total number of deaths come from long-term care facilities. As of now, that number has climbed another five percentage points on a national level. Some individual states have it much worse than the national average.
Last Tuesday, Pennsylvania released an assessment of its COVID-19 numbers, detailing, among other things, every coronavirus case on record in their long-term stay facilities. According to the Pennsylvania National Electronic Disease Surveillance System (PA-NEDSS), there are a reported 2,852 deaths across 558 nursing homes statewide. And while some nursing homes have managed to get away without having a single case, others, such as Northampton Country Home in Gracedale, have seen as many as 205 cases and 44 deaths at a single facility. Either way, deaths in nursing homes have hit Pennsylvania disproportionately. As of May 19, the state’s total number of deaths was 4,624, making long-term nursing facility patients upwards of 60 percent of total COVID-related deaths in the state.
New Jersey has reported cases of coronavirus in up to 80 percent of all of its nursing home facilities. And between March 1 and May 1, the state of New York lost more than 4,800 elderly citizens in nursing homes, prompting Gov. Andrew Cuomo to call extended-stay facilities “feeding frenzies” for the virus.
A Familiar Crisis on a Bigger Scale
A 2008 study from the Journal of Post-Acute and Long-Term Medicine found that 20 to 24 percent of all deaths in the United States occurred in nursing homes. Of those, 23 percent were caused by pulmonary or respiratory complications.
Another study from JAMDA in 2015 found similar results concerning length of stay. The study found that nearly 12 percent of residents in long-term care facilities died after one year of admission. About a quarter of first-year residents were hospitalized at least once.
So what makes COVID-19 so detrimental to nursing homes isn’t only its mortality rate, but rather also its ability to spread as aggressively among a particularly susceptible population.
Efforts to stop the spread have not failed for a lack of trying. Both the Centers for Medicare and & Medicaid Services (CMS) and the Centers for Disease Control and Prevention (CDC) released guidelines on how to respond to COVID in nursing homes. The CDC in particular issued numerous resources such as their Key Strategies for Long-Term Care Facilities, the Infection Prevention and Control Assessment Tool for Nursing Homes Preparing for COVID-19, and the Strategies to Mitigate Healthcare Personnel Staffing Shortages. Each one of these resources provides extremely detailed procedures in an attempt to facilitate the fight against coronavirus for nursing home leadership. Many of these procedures aren’t new novel instructions.
Viruses aren’t a new to nursing homes either. Each year, nursing homes have to be very careful of viruses that could affect their residents. The spread of norovirus, a highly contagious gastrointestinal virus, posed a serious concern to many in the long-care industry—especially between the years of 2009 and 2012. While the threat posed by norovirus was significantly lower than coronavirus, many of the methods of preventing norovirus are similar to the procedures and methods to stop COVID, including techniques like isolation and distancing between patients. But even with these practices in place, virus management is only half of the problem.
Mixed Signals and Instructions
Despite pre-existing and new guidelines, critical decisions made by governors and state leadership have, in some cases, exacerbated the crisis. In New York, Gov. Cuomo’s instruction for long-term care facilities to continue accepting patients with COVID-19 led to devastating results. His mandate came after the Society for Post-Acute and Long-Term Care Medicine (ADMA) issued a warning about transferring coronavirus patients in and out of nursing home facilities. In their brief titled, “Transfer of Hospital Patients to PALTC settings,” ADMA explicitly laid out the dangers presented by COVID exposure to care facilities:
“Unsafe transfers will increase the risk of transmission in PALTC facilities, which will ultimately only serve to increase the return flow back to hospitals, overwhelming capacity, endangering more healthcare personnel, and escalating the burden on hospitals,” ADMA experts said.
AMDA further laid out that nursing homes should not accept COVID patients and that an infected patient discovered on the premises should be carefully separated from other residents.
As a result of climbing losses, Cuomo has since rescinded his mandate, but not before garnering backlash for the decision. Many like Janice Dean, a meteorologist for Fox News, blame the governor’s decision for the death of elderly loved ones.
In Michigan, Sen. Peter Lucido is calling for an investigation from the Attorney General and the U.S. Attorney into why Gov. Gretchen Whitmer forced nursing homes to accept COVID-positive residents, in an order similar to Cuomo’s. Whitmer denies the claims, saying that her mandate made no such thing explicitly mandatory, but with over 2,300 cases of coronavirus presently in Michigan nursing homes, her critics aren’t swayed by the explanation.
“Why would you want to bring an infected COVID patient into a nursing home where the most vulnerable people in the state are living?” Lucido asked ABC news.
Uncertainty of Scale
As devastating as the numbers are, part of the problem with addressing the COVID-19’s impact on nursing homes is the uncertainly of cases reported. The numbers could be higher.
Only in the past week have the CDC and healthcare provides required nursing homes to record and report cases. Up until this point, individual nursing homes may have been keeping track of cases, but not in a required format. Medicare and Medicaid have put out a set of requirements that, going forward, will call for specific numbers that started Sunday, May 24. Facilities that don’t start reporting until May 31 will receive a warning notice from the CDC for violating of the mandate.
The instructions come along with the CDC-issued “Human Infection 2019 Novel Coronavirus Case Report Form.” The new form includes case classification and verification, hospitalization and ICU details, case demographics, exposure information, and clinical symptom history. These measures aim to pin down the patterns and elements having an impact on a nursing-home population.
But with more than two months of crisis already in the books, experts like Thomas Perls, a Professor of Medicine at Boston University, believe this mandate comes too late to assure accurate and reliable reporting.
Perls notes that a lack of systemic case tracking—specifically in nursing homes—has been a trend in other countries as well, one that’s allowed additional infection to sneak under the radar.
“The missing cases [in nursing homes] could dramatically skew the national death count.” Perls said. “When France started reporting death data from some of its nursing homes, the daily COVID-19 fatality numbers almost doubled.”
The Trump Administration decided it will not require long-term care facilities to report numbers of cases prior to May 6. Perls’ concern is that too many cases have slipped through for the United States to have a comprehensive understanding of the area of effect the virus has had on long-term care facilities even after the implementation of a report requirement.
Depleted nursing staffs, struggling to keep their heads above water, will also make gathering an accurate county unlikely. According to PBS news, it’s not just the patients that are struggling. Staff shortages due to COVID-19 directly impact residents, leaving many without the attention they need on a daily basis.
Charlene Harrington, a professor at the University of California, San Francisco and an expert in nursing home services, told CBS News that part of the problem is a lack of resources—both in terms of a qualified workforce and medical capacity.
“Before the pandemic, 75 percent of the nursing homes did not have enough staff, especially registered nurses,” Harrington said, “and registered nurses are essential for infection control, for assessing residents and managing the staff in nursing homes.”
Now exacerbated by the crisis, a lack of trained professionals is translating to a lack of comprehensive tracking inside long-term care facilities and a loss of life.