Despite media hype and the claims of flashy press releases, there is currently no single test or tool that can accurately diagnose Alzheimer’s disease or predict with 100 percent certainty who will develop it — or any of the other similar neuro-degenerative diseases. Further, tests being marketed directly to consumers can have high false-positive results, implying a person has the disease when they do not.
The repercussions of these inaccurate tests can be detrimental to one’s mental health, but consumer access to genomic and DNA testing is beginning to show us that no matter what, people want to probe this kind of information, and that test conclusions will result in all kinds of moral dilemmas.
Technology is getting us closer and closer to where we can not only test our ancestry with the likes of 23andMe, Ancestry.com, MyHeritage, or Helix, but also our disease propensity. A simple blood test or DNA sample could soon inform us what will happen if the right combination of factors play out in our lives and we live long enough.
But as humans become more comfortable with at-home testing kits and with allowing companies to assess their biological makeup, the variety of tests available and amount of information shared will undoubtedly grow. This should frighten us for a number of reasons, ranging from emotional distress caused by unexpected results (see what 23andMe was dealing with during Christmas) to privacy concerns, to long-term care insurance ramifications.
However, it is most important to remember that currently available tests are not as advanced — or accurate — as they often claim to be, and don’t reveal everything a consumer might want. When medical professionals are asked about the at-home tests, they often tell patients the best one to buy really depends on what you want to know and, even then, the results should be taken very lightly, as they merely let you know that you are “at risk” for a disease or disorder.
Do You Really Want to Know?
The Alzheimer’s Association contends that early and accurate diagnosis of Alzheimer’s could save an estimated $7.9 trillion in medical and care costs, and that in 2018 alone, Alzheimer’s and other dementias will cost the U.S. $277 billion, with a new diagnosis occurring as frequently as every 65 seconds. But these population-level numbers only tell a part of the story. When 10 percent of people older than 65 have Alzheimer’s — and that cohort is steadily growing — the toll taken on families is immeasurable.
With nearly one in every five Medicare dollars spent on dementia, the need for testing and therapies is great. But testing is not a cure. Therapies are not a cure. Would you really want to know if you are going to develop, or are already in pre-symptomatic early stages of, Alzheimer’s disease? There is currently no known cure and only marginal progress in symptomatic treatments.
In fact, the reason a disease like Alzheimer’s is such a compelling “what if” scenario for genetic testing is that the results may change the way one behaves and plans for the future, but they can’t be undone. Would individuals or families really make different life choices? We know smoking and obesity kill millions of Americans each year, yet those behaviors persist. Perhaps it is true that ignorance is bliss.
Biomarkers and genetic testing for cancer, diabetes, heart disease, and other chronic diseases will not introduce the same level of intergenerational stress and concern for families as neurological and degenerative conditions like dementia. And so long as potential cure after potential cure fails in clinical trials, the medical community will call the ethics of such tests into question, and the lay community will continue to make ill-informed decisions based on insufficient information.
The Future Is Bright, But Uncertain
The dichotomy of those who want to know and those who do not is separated by a deep chasm in personal history and belief systems, and could forever alter the way individuals, families, and society prepare for disease, as well as how insurers, care providers, and employers provide and pay for care. It could also eventually result in drastic changes in decision-making for family planning and societal implications of who should and should not receive care based on their risk. While genetic tests are presently able to determine thousands of diseases and disorders, in-home tests are limited by the Food and Drug Administration to about 10 diseases and conditions.
But a breakthrough with 100 percent accuracy for predicting a degenerative disease like Alzheimer’s could have unprecedented impact on behaviors and costs to society, actually bending the cost curve health experts so often talk about as necessary for economic stability. With that said, the unintended consequences of such information must be explored in advance.
Shifts in care provider workforce and insurance markets could be drastic. Without a cure, likely new models for saving for retirement will be created. This is because at present, long-term care insurance, disability insurance, and life insurance can prohibit you from coverage if your genetic tests show a propensity for Alzheimer’s.
Congress did take a major step forward in protecting patient privacy for genetic testing by passing the 2008 Genetic Information Nondiscrimination Act (GINA), which protects Americans from being discriminated against by an employer or health insurer based on genetic information. However, the concerns about privacy and decision-making do not end with GINA. Since 2017, when 23andMe partnered with GlaxoSmithKline, the world learned that genetic testing companies and pharma always planned to link.
In this particular case, 23andMe gained a $300 million investment, and GSK — along with six other pharma companies 23andMe made deals with — gets all of the consenting patients’ behavioral, health, and genetic information. The obvious goal is drug R&D and drug targeting to specific individuals. But with many not knowing that their spit sample or blood test results are being sold to third-parties for large sums of money and targeting, privacy issues are certain to mount in the coming years as disease knowledge gets more accurate and more serious.
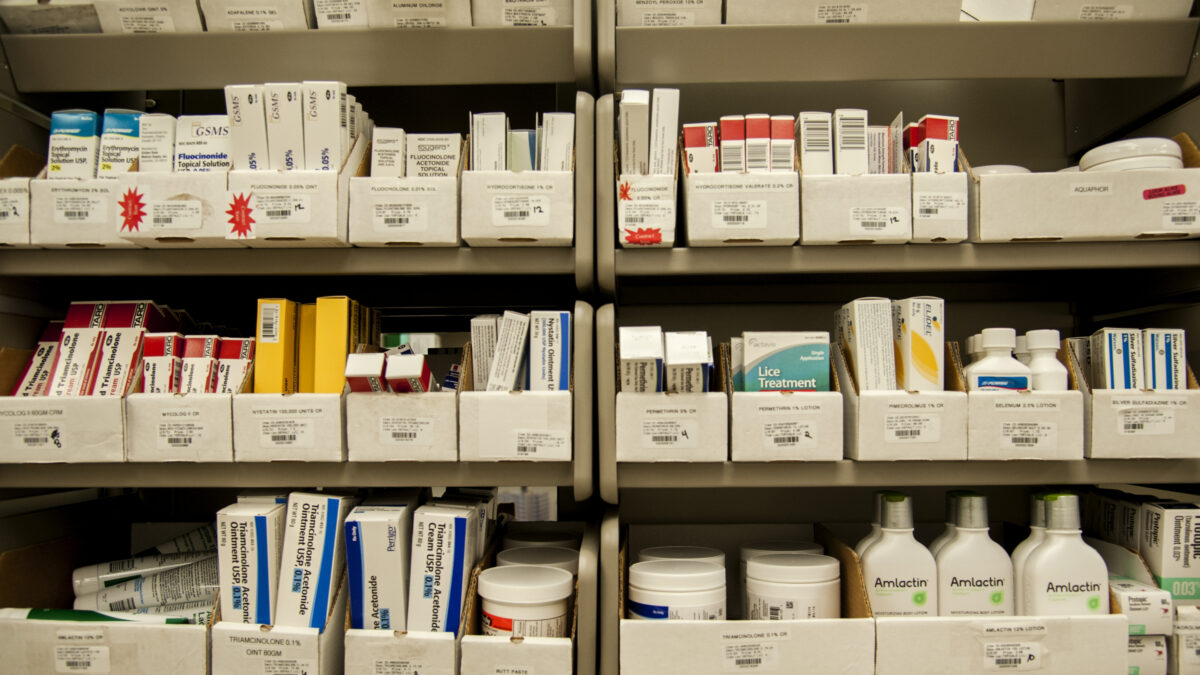
While CVS and Walgreens’ shelves are not presently stocked with 100 percent accurate genetic tests, it may not be long before in-clinic and in-home testing is available to consumers. But without a cure or highly effective symptomatic treatments to go hand-in-hand with genetic testing, the results will certainly take a toll on individuals, families, health care markets, and communities — and require a lot more genetic counselors.
If you do decide to receive genetic testing, particularly for risk factors for Alzheimer’s and other neurodegenerative diseases, here is some added information and advice from the Mayo Clinic.